Radiculopathy
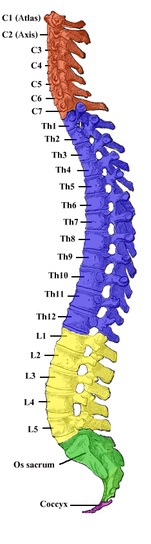
Radiculopathy is a condition that involves irritation of the spinal nerves, the roots of those nerves, or both. It most commonly occurs as a result of spondylosis or disc pathology.
Epidemiology: The frequency of radiculopathy increases with age, slightly more commonly in men than in women. Cervical radiculopathy is less common than lumbar radiculopathy.
Symptoms: Acute, radiating pain along the course of the nerve to the shoulder, arm, or hand in the case of cervical radiculopathy (brachialgia) or to the buttock, thigh, calf, or foot in the case of lumbar radiculopathy (sciatica), sensory disturbances, and muscle weakness.
Diagnosis: Diagnostic imaging such as MRI or CT scan is used, along with a detailed patient history. A thorough physical examination is also necessary, assessing muscle strength, superficial sensation, and neurological reflexes.
Treatment: The treatment of radiculopathy aims to initially “calm down” the irritated nerve. This can be achieved through properly tailored exercises, manual therapy (mobilizations, tractions, neurodynamics, soft tissue work), physical therapy (electrotherapy, ultrasound, laser therapy), kinesiotaping, and patient education. In the acute phase, the patient is often supported with analgesic and anti-inflammatory medications. Surgical treatment is considered when conservative treatment has been used for a longer period without desired effects or when extremely large impairments occur.
Scheuermann’s Disease (Juvenile Kyphosis)
In Scheuermann’s disease, the vertebrae undergo deformation, taking on a wedge shape. This results in changes in the curvature of the spine. There is an increased kyphosis of the thoracic spine and stiffness in the thoracic region.
Epidemiology: It most commonly affects adolescent boys, but can also occur in young girls aged 11-18 years. The first symptoms can be observed during puberty, although cases have been reported as early as 9 years of age. The literature suggests that this condition affects 0.5-8% of the population. The exact causes are not fully understood, but genetic factors are believed to have the greatest influence.
Symptoms of Scheuermann’s Disease: Back pain, a “slouched” posture with rounded back, forward head and shoulders, tilted shoulder blades, compensatory hyperlordosis in the lumbar and cervical regions, protruding abdomen, anterior pelvic tilt, barrel-shaped/pectus excavatum chest, lateral spinal curvature, stiffness of the spine (especially in the thoracic region), circulatory and respiratory disturbances, and neurological symptoms (weakness in the lower extremities, radicular pain).
Diagnosis: The diagnosis of Scheuermann’s disease involves taking a patient history, conducting a physical examination, and using X-rays to assess the spinal structures in detail. Additionally, the Risser test (which evaluates skeletal maturity), clinical tests, goniometric measurements, and spirometry may be used. Diagnosis can also be complemented with MRI and bone scintigraphy.
Treatment of Scheuermann’s Disease: n the early stages of the disease, conservative treatment is typically employed whenever possible. This includes corrective exercises, bracing (for more severe cases), physiotherapy, and patient education. Surgical treatment is rarely employed and is reserved for cases with significant deformity that causes debilitating and restrictive symptoms.
Untreated or late-diagnosed Scheuermann’s disease can lead to the development of early degenerative changes in the spine and chest.
Stress Fracture of the Vertebra
Unlike normal fractures that occur as a result of trauma, stress fractures occur due to the accumulation of micro-damage in the bone. In such fractures, the bone is subjected to high loads over a long period of time, and the tissue fails to keep up with the rebuilding process.
Epidemiology: Stress fractures most commonly occur in professional athletes and military personnel. Additional risk factors include alignment disorders, metabolic disorders, osteoporosis, osteopenia, poor diet, impaired blood flow, and being female. In terms of sports, athletes in disciplines such as gymnastics, ballet, volleyball, diving, soccer, and cricket are most at risk.
Symptoms of a stress fracture of the vertebra: Pain not caused by any trauma, tenderness, mild warmth, and swelling at the fracture site. The pain often occurs at the end of a training session or after its completion. Because the discomfort is not severe, patients often seek medical attention after several weeks. Over time, the pain gradually increases.
Diagnosis: MRI is the most accurate diagnostic tool for evaluating stress fractures. Changes may not be visible on X-rays for 2-8 weeks after the onset of symptoms. Initially, an ultrasound scan can be performed as it is a cheaper imaging study that can also detect signs of overload in the affected area. Besides imaging studies, an orthopedic specialist conducts a thorough patient history and clinical examination. It is often observed that the patient started more intense training a few weeks prior.
Note: The provided translation is for informational purposes only and should not be relied upon as a substitute for professional medical advice.
Treatment of stress fracture of the vertebra: Patients are typically advised to take a break from physical activity for about 8 weeks, although low-impact exercise that does not overly stress the affected area is allowed. Physical therapy interventions such as magnetic field therapy and cold packs may be recommended. Surgical treatment is performed when there is no bone union or delayed bone union, or when a complete fracture occurs.
You’re welcome!